| єя«•«ьљƒ : ∆чљЇ≈Ќ
|
ЅҐЉцєш»£ - 540257 25 |
| Initial Loading Therapy of Cilostazol Improved Antiplatelet Responsiveness in Patients with Percutaneous Coronary Intervention |
| лПЩмХДлМАнХЩкµР мЭШк≥ЉлМАнХЩ мИЬнЩШкЄ∞лВік≥Љ¬є мІДлЛ®к≤АмВђмЭШнХЩк≥Љ¬≤ , лґАмВ∞лМАнХЩкµР мЭШк≥ЉлМАнХЩ мИЬнЩШкЄ∞лВік≥Љ¬≥ |
| л∞±нЭђк≤љ, кєАлђінШД¬є , мЦіл£°нШЄ¬є , м°∞мЪ©лЭљ¬є , мЮ•нЩНм≤†¬є , мЭім£ЉмШБ¬є , л∞ХнГЬнШЄ¬є , кєАмШБлМА¬є , к≥†л¶ђмШБ¬≤ , нХЬмІДмШБ¬≤ , м∞®кіСмИШ¬≥ |
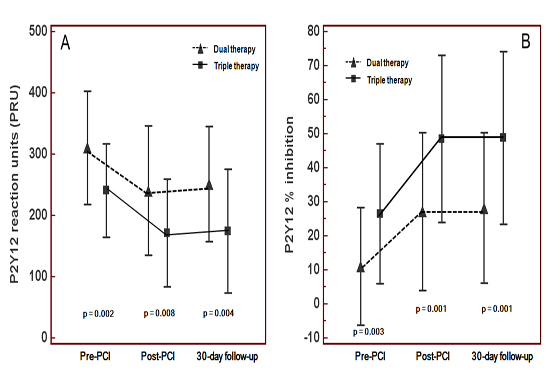
Background and Objectives: To date, most of studies are retrospective or prospective study conducted with cilostazol as an agent of maintenance dose therapy, a few data has been reported the loading dose (LD) effects of cilostazol on platelet inhibition in patients undergoing percutaneous coronary intervention (PCI). We sought to investigate the role of adjunctive LD of cilostazol in platelet reactivity post-treatment. Subjects and Methods: Sixty consecutive patients undergoing PCI were enrolled and assigned to receive 300-mg LD of aspirin and clopidogrel with or without 200-mg LD of cilostazol. All of LD were given at least 3 hours before PCI and followed by dual or triple maintenance dose (MD) therapy. Platelet function tests were performed at just before the procedure, 24 hours and 30 days after PCI using light transmittance aggregometry (LTA) and VerifyNow P2Y12 assay. Results: Comparing baseline and angiographic characteristics between two groups, there were no significant differences. In the pre- and post-procedural phases (24 hours and 30 days after PCI), the triple LD/MD therapy significantly reduced the mean PRU-value (Fig. 1) and ARU-value (476.7¬±92.5 vs. 410.9¬±61.0, p = 0.002; 465.0¬±72.9 vs. 420.2¬±48.9, p = 0.007; and 475.1¬±57.6 vs. 410.7¬±51.7, p = 0.129, respectively) and increased the average of P2Y12 % inhibition than the dual LD/MD therapy (p <0.01). In the LTA tests, the triple LD/MD therapy versus the dual LD/MD therapy also revealed significant reduction of 10 µM ADP-induced MPA in the pre- and post-procedural phases, except for 0.5 mM AA-induced MPA. Cilostazol significantly reduced the incidence of high post-treatment platelet reactivity (HPPR). Conclusions: Adjunctive LD of 200-mg cilostazol can improve platelet responsiveness to clopidogrel in the pre-procedural as well as post-procedural phase, reducing the prevalence of HPPR.
Key words: Cilostazol, Platelet function tests, Drug-eluting stents
|
|
|
Warning: getimagesize(/home/virtual/circulationadmin/renewal/econgress/conference/abstract/img_files/Figure1A.jpg) [function.getimagesize]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/econgress/conference/manage/schedule/view_abstract.php on line 164
|
|





