| єя«•«ьљƒ : ±Єњђ
|
ЅҐЉцєш»£ - 540579 188 |
| Is The Formation of Lipid-rich Plaque in the Neointima Related to Development of Very Late Stent Thrombosis after Implantation of Drug-Eluting Stent?: Optical Coherence Tomography Analysis of Stent Thrombosis and In-stent Restenosis |
| мЧ∞мДЄмЭШлМА мЛ†міМмДЄлЄМлЮАмК§л≥СмЫР ¬є , к≤љнЭђлМАнХЩкµР лПЩмДЬмЛ†мЭШнХЩл≥СмЫР¬≤ , мХДм£ЉмЭШлМАл≥СмЫР¬≥ , мЧ∞мДЄмЭШлМА мЫРм£ЉкЄ∞лПЕл≥СмЫРвБі |
| кєАлПЩлѓЉ¬є, к≥†мШБкµ≠¬є , м°∞мІДлІМ¬≤ , мµЬмЖМмЧ∞¬≥ , мЬ§м†ХнХЬвБі , кєАм§СмД†¬є , мµЬлПЩнЫИ¬є , нЩНл™ЕкЄ∞¬є , мЮ•мЦСмИШ¬є |
Background
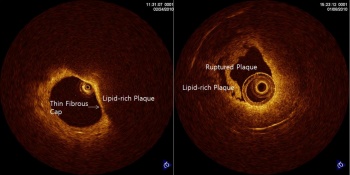
Very late stent thrombosis (VLST) after implantation of drug-eluting stent (DES) is generally thought to be caused by incomplete surface coverage of stent struts and late malapposition. Lipid-laden neointima and rupture of lipid-rich plaque (LRP) may be possible causes of VLST after implantation of bare metal stent (BMS). However, whether formation of LRP also contributes to development of VLST after implantation of DES is unknown.
Methods
We analyzed OCT images of 18 patients who developed stent thrombosis after implantation of DES and OCT images of 32 patients with DES in-stent restenosis from the Yonsei OCT registry. We investigated whether features of plaque rupture (PL) and LRP within neointima were present on OCT images and review clinical and procedural data of the patients.
Results
Of the 18 patients with stent thrombosis, 4 patients (22.2%) showed plaque rupture on OCT images. Mean follow-up duration was significantly longer in the PL+ group (45.4±19.3 months vs 29.5±18.1 months, p-value=0.15) than PL- group. LRP was also more frequently observed in the PL+ group. Incidence of uncovered struts (0.0% vs 64.2%, p-value=0.08) and stent malapposition (0.0% vs 57.1%, p-value=0.09) were not shown in PL+ group.
Among 32 patients with ISR, 5 patients (15.6%) showed LRP on OCT images. Mean angiographic follow-up duration was significantly longer in the LRP+ group (29.2±22.0 months vs 11.1±5.6 months, p-value=0.02) than LRP- group. Lesion diameter and length was larger and shorter in the LRP+ group than LRP- group (diameter: 3.2±0.28 vs 2.9±0.24 p-value=0.02, length: 23.5±5.2 vs 29.0±4.9 p-value=0.04).
Conclusions
PR was identified in a small group of patients with VLST after implantation of DES. LRP was also observed inside the stents in some patients with stent thrombosis and ISR. This observation suggests the formation of LRP within the neointima inside DES may contribute to development of VLST in some patients. The link between presence of LRP and VLST needs to be validated in further studies.
|
|
|
Warning: getimagesize(/home/virtual/circulationadmin/renewal/econgress/conference/abstract/img_files/Picture-resizing1.jpg) [function.getimagesize]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/econgress/conference/manage/schedule/view_abstract.php on line 164
|
|





