| єя«•«ьљƒ : ±Єњђ
|
ЅҐЉцєш»£ - 550621 59 |
| Long-term clinical outcome and its predictors of cardiac mortality in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction |
| мДЬмЪЄлМАнХЩкµР л≥СмЫР¬є , лґДлЛємДЬмЪЄлМАнХЩкµРл≥СмЫР¬≤, м†ДлВ®лМАнХЩкµРл≥СмЫР¬≥, нХЬл¶ЉлМАнХЩкµРл≥СмЫР вБі , нХЬмЦСлМАнХЩкµРл≥СмЫР5, мґ©лВ®лМАнХЩкµРл≥СмЫР6 |
| л∞ХнШДмЫЕ¬є, мЬ§м∞љнЩШ¬≤ , мДЬм†ХмЫР¬≤, мХИмШБкЈЉ ¬≥, нХЬкЈЬл°Э вБі, кєАмИЬкЄЄ 5 , мД±мЭЄнЩШ6 , мµЬлПЩм£Љ¬≤, and KORMI investigators |
Background-There has been controversy over the disparity between ST-segment elevation myocardial infarction (STEMI) and Non-STEMI (NSTEMI) in the long-term mortality and predictors of cardiac mortality. The aim of this study was to compare clinical outcome and prognostic factors of STEMI and NSTEMI.
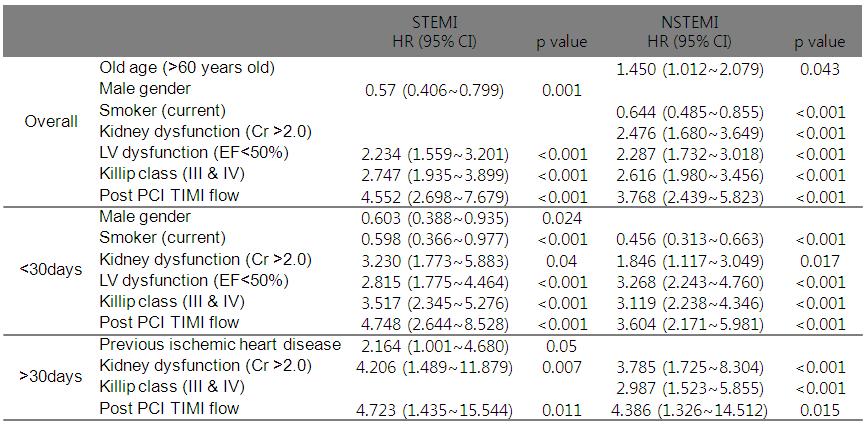
Methods and Results-We extracted 8293 patients who were hospitalized for STEMI (n=4843) and NSTEMI (n=3450) between November 2008 and September 2010 from the nationwide registry of Korea Working Group of Myocardial Infarction (KorMI). We analyzed major adverse cardiac events (MACE) in patients with STEMI and NSTEMI during clinical follow-up for more than 1 year. As compared to patients with STEMI, those with NSTEMI were older, and showed higher prevalence of hypertension, diabetes mellitus, dyslipidemia, prior ischemic heart disease, and left ventricular (LV) systolic dysfunction. Early revascularization was performed 97% in patients with STEM and 77% in patients with NSTEMI.Mortality occurred in 421 patients (8.7%) in STEMI and 190 patients (5.5%) in NSTEMI during follow up. Landmark analysis showed cardiac mortality was significantly higher in patients with STEMI compared to those with NSTEMI during the first 30 days, but no difference in mortality rate between the two groups afterwards. Hazard ratio for cardiac death during the first 30 days was significantly higher in patients with STEMI (adjusted HR 1.75; 95% CI, 1.30~2.36, p<0.001), but hazard ratio from 30 days were not different between STEMI and NSTEMI. Neither risk for repeated myocardial infarction nor risk for target lesion revascularization was not different between STEMI and NSTEMI. Before and after 30 days, some different independent predictors was revealed between STEMI and NSTEMI.
Conclusion STEMI was associated with a higher risk of short-term mortality, but both STEMI and NSTEMI showed comparable long-term mortality after 1 month. Different prognostic factors should be used to assess the risk for cardiac mortality in STEMI and NSTEMI.
|
|
|
Warning: getimagesize(/home/virtual/circulationadmin/renewal/econgress/conference/abstract/img_files/1.jpg) [function.getimagesize]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/econgress/conference/manage/schedule/view_abstract.php on line 164
|
|





