| єя«•«ьљƒ : ±Єњђ
|
ЅҐЉцєш»£ - 550937 77 |
| Unprotected Left Main Stenting with Everolimus-Eluting Stent: PRECOMBAT-2 Study |
| ¬ємЪЄмВ∞лМАнХЩкµР мДЬмЪЄмХДмВ∞л≥СмЫР, ¬≤мЧ∞мДЄлМАнХЩкµР, ¬≥м†ДлВ®лМАнХЩкµР, вБімДЬмЪЄлМАнХЩкµР, 5к≥Дл™ЕлМАнХЩкµР, 6к≥†л†§лМАнХЩкµР кµђл°Ьл≥СмЫР, 7к≥†л†§лМАнХЩкµР мХИмХФл≥СмЫР, 8к∞АнЖ®л¶≠лМАнХЩкµР, 9лґАмВ∞лМАнХЩкµР, 10мЪЄмВ∞лМАнХЩкµРл≥СмЫР, 11к≤љлґБлМАнХЩкµР, 12мД±кЈ†кіАлМАнХЩкµР |
| л∞ХмКєм†Х¬є , кєАмШБнХЩ¬є ,л∞ХлНХмЪ∞¬є ,мЬ§мД±м≤†¬є ,мХИм†ХлѓЉ¬є ,мЖ°нШЬкЈЉ¬є ,мЭімҐЕмШБ¬є ,кєАмЫРмЮ•¬є ,к∞ХмИШмІД¬є ,мЭімКєнЩШ¬є ,мЭім≤†нЩШ¬є ,л∞ХмД±мЪ±¬є ,мЮ•мЦСмИШ¬≤ ,м†Хл™ЕнШЄ¬≥ ,кєАнЪ®мИШвБі,нЧИмКєнШЄ5,лВШмКємЪі6,мЮДлПДмД†7,мКєкЄ∞л∞∞8, кєАм§АнЩН9, мЭімГБк≥§10,л∞ХнЧМмЛЭ11,кґМнШДм≤†12 |
Background: The PRECOMBAT randomized study showed a non-inferiority of percutaneous coronary intervention (PCI) with the first-generation sirolimus-eluting stent (SES) for unprotected left main coronary artery (ULMCA) stenosis compared with coronary artery bypass graft surgery (CABG) with regard to the incidence of 1-year major adverse cardiac and cerebrovascular events (MACCE) including death, myocardial infarction (MI), stroke or ischemia-driven target vessel revascularization (TVR). However, the efficacy of the second-generation drug-eluting stent for such a lesion is not known well.
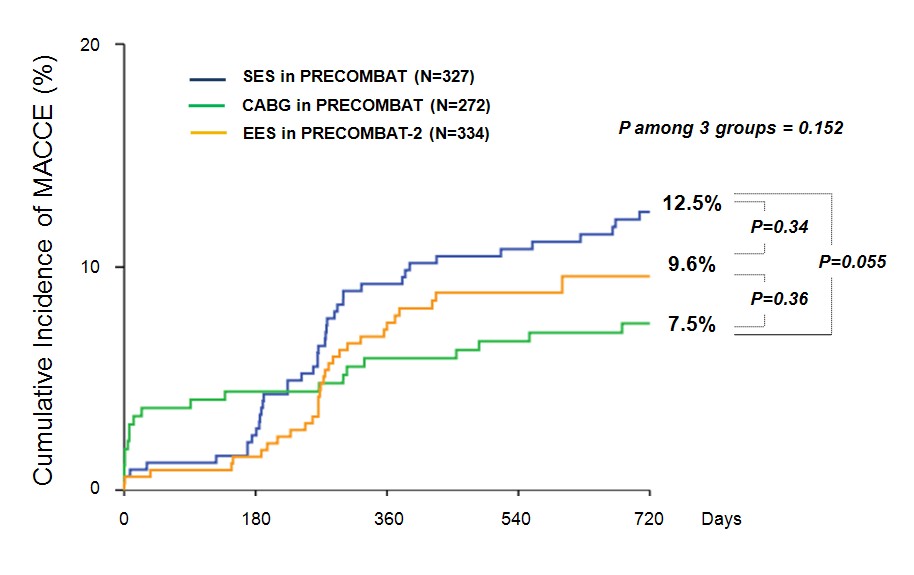
Method: The PRECOMBAT-2 study prospectively enrolled 397 consecutive patients who received PCI with everolimus-eluting stent (EES) for ULMCA stenosis. From this registry, the outcomes of 334 (84.1%) patients meeting the randomization criteria of the PRECOMBAT study were compared with those of patients randomized to SES (N=327) and CABG (N=272) in the PRECOMBAT study. The primary end point was the rate of MACCE over 2 years.
Results: Baseline clinical characteristics were well matched among the 3 groups. However, angiographic follow-up was less frequently performed in the EES than in the SES group due to the less obligatory recommendation (60.8% vs. 76.1%, p<0.001). The MACCE rate over 2 years did not differ significantly among the 3 groups as shown in Figure. The 2-year incidences of composite of death, MI or stroke also did not differ among SES, EES and CABG groups (3.3% vs. 4.4% vs. 4.8%, p among the 3 groups=0.70). However, the incidence of ischemia-driven TVR was lower in the CABG (3.4%) than in the EES (7.2%) or SES (9.2%) groups (p among the 3 groups=0.023). Between the EES and SES groups, the incidences of MACCE and any individual end points were not different over 2 years.
Conclusions: EES showed a similar efficacy for the treatment of ULMCA stenosis, as compared with PCI with SES or CABG, with regard to the incidence of MACCE over 2 years.
|
|
|
Warning: getimagesize(/home/virtual/circulationadmin/renewal/econgress/conference/abstract/img_files/MACE1.jpg) [function.getimagesize]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/econgress/conference/manage/schedule/view_abstract.php on line 164
|
|





