 Intervention of the Month Intervention of the Month |
|
| Very Late Stent Thrombosis due to Neointimal Plaque Rupture 6 Years after Paclitaxel-Eluting Stent Implantation |
Won Ju Kee, MD, Min Goo Lee, MD, Keun-Ho Park, MD, PhD, Doo Sun Sim, MD, PhD, Young Joon Hong, MD, PhD, Ju Han Kim, MD, PhD, Youngkeun Ahn, MD, PhD, FACC, FSCAI, and Myung Ho Jeong, MD, PhD, FACC, FAHA, FESC, FSCAI
The Heart Research Center of Chonnam National University Hospital, Gwangju, Korea
|
|
A 39-year-old male underwent coronary stent implantation for stable angina pectoris in September 2004. Risk factor included only hyperlipidemia. The patient had thrombotic near total occlusion of the mid right coronary artery (Type C, 99%, TIMI flow I) (Fig 1A) and critical stenosis of the mid left anterior descending artery (Type B2, 90%, TIMI flow III) (Fig1C). After intracoronary administration of a glycoprotein IIb/IIIa inhibitor (ReoPro®), percutaneous transluminal coronary angioplasty (PTCA) using 3.5mm balloon was performed, and there was placement of a 3.5x32mm paclitaxel-eluting stent (Taxus Express², Boston Scientific Corporation) in the RCA (Fig 1B) and a 3.0x20mm Taxus-eluting stent in the LAD (Fig 1D). He was compliant with his medications which were aspirin 100mg, clopidogrel 75mg, cilostazol 200mg, carvedilol, losartan, ezetimibe, simvastatin and isosorbide dinitrate. In February 2005, coronary angiogram was performed again because of mild chest pain and showed no in-stent restenosis in both coronary arteries (Fig 2A and B). Cilostazol was stopped 6 month after drug-eluting stent implantation. He was continued on medication of dual anti-platelet agent for 5 years. In follow-up with the patient, two- dimensional echocardiogram showed no regional wall motion abnormality with 69.4% of ejection fraction and the treadmill test was negative at 12.8 METS.
The patient presented to the emergency room with sudden, left-sided chest pain without radiation in October 2010. A 12-lead EKG showed ST-segment elevation in the II, III, aVF and type II second degree AV block (Fig 3). He was found to have a normal complete blood count, with white blood cell count of 5,900/mm3 hemoglobin of 13.8 g/dL, hematocrit of 41.1%, and platelet count of 199,000/mm3. The results of electrolyte panel, kidney function studies, liver function studies, and lipid panel were all within normal limits except for the LDL of 86 mg/dL. Cardiac enzymes were initially normal.
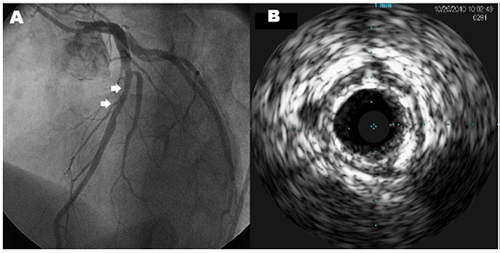
The patient underwent cardiac catheterization and it revealed stent thrombosis in RCA (99%, I, 0) (Fig 4A) and mild type II ISR in LAD (40%, III, 0) (Fig 5). Intravascular ultrasound (IVUS) showed neointima breakdown and ruptured plaque in the RCA stent (Fig 4B). We performed plain old balloon angioplasty (POBA) with 3.5x15mm balloon for RCA and final CAG and IVUS showed good distal flow and markedly decreased residual stenosis (Fig 4C and D). He was found to be hyporesponsive to clopidogrel when tested for adenosine diphosphate (ADP)-induced platelet aggregation utilizing the Verify Now P2Y12 point-of-care assay (301/14 P2Y12 reaction unit/%). He was discharged after uneventful recovery with triple anti-platelet therapy using aspirin 100 mg, clopidogrel 75 mg, cilostazol 200 mg daily. The patient has been followed up at the outpatient department without further symptoms.
Although the mechanisms of late stent thrombosis have not been completely understood, it is presumed that delayed endothelialization, chronic inflammation, hypersensitivity to the polymer, initial or acquired stent mal-apposition, residual reference segment stenosis and penetration of necrotic core may play a role. Furthermore, non-responsiveness to clopidogrel is associated with higher risk of cardiovascular events, including cardiac death and stent thrombosis. The prevalence of clopidogrel resistance in the patient population was reported in the range of 5 to 44%. We can conclude that very late stent thrombosis may indeed occur in clinically stable patients while on dual anti-platelet therapy, as the multiple factors can influence the pathological mechanisms of late thrombosis.
|
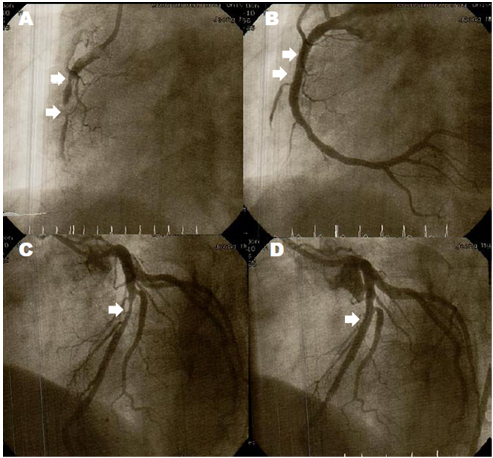 |
▲ Figure 1. Initial coronary angiography in September 2004. A: Thrombotic near total occlusion of the mid RCA (Type C, 99%, TIMI flow I). B: 3.5x32 mm paclitaxel-eluting stent (Taxus Express², Boston Scientific Corporation) was deployed in RCA. C: Critical stenosis in mid LAD. (Type B2, 90%, TIMI flow III) D: 3.0x20 mm Taxus-eluting stent in the LAD. Final CAG showed good distal flow without residual stenosis.
|
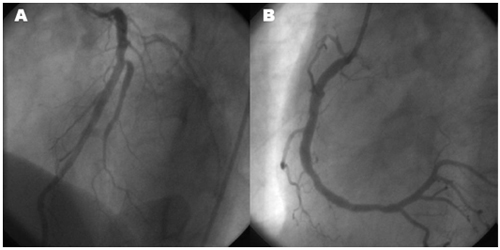 |
▲ Figure 2. Coronary angiography performed in February 2005. No in-stent restenosis in LAD (A) and RCA (C) stents on follow-up coronary angiogram.
|
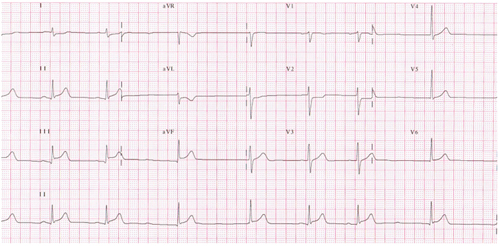 |
▲ Figure 3. A 12-lead EKG showed ST-segment elevation in the II, III, aVF and type II second degree AV block.
|
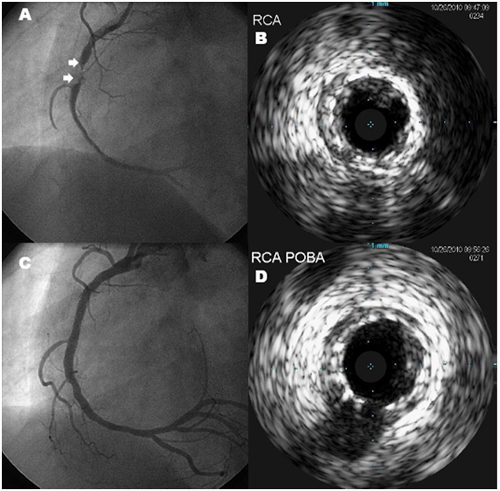 |
▲ Figure 4. A : Right coronary angiogram showed very late stent thrombosis in RCA stent. B: IVUS showed neointima breakdown and ruptured plaque within the RCA stent. C: Coronary angiography after plain old balloon angioplasty (POBA). Final coronary angiogram showed good distal flow D: IVUS showed markedly decreased residual stenosis.
|
 |
▲ Figure 5. A : Left coronary angiography showed mild type II in-stent restenosis in LAD. B : IVUS showed plaque in LAD stent.
|
|
| |
위의 이달의 중재술을 보신 선생님들의 의견을 아래의 의견 쓰기에 의견을 남겨 주십시오.
선생님들의 다양한 의견을 받습니다.
|
![[의견쓰기]](/image/comment_btn.gif) |
Warning: include(/home/virtual/circulationadmin/new/info/comment_index.php) [function.include]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/info/case/201012/case201012.htm on line 171
Warning: include() [function.include]: Failed opening '/home/virtual/circulationadmin/new/info/comment_index.php' for inclusion (include_path='.:/usr/local/php/lib/php') in /home/virtual/circulationadmin/new/info/case/201012/case201012.htm on line 171
|
|
|