|
 Case Case
|
A 74-year-old man was referred to the emergency room for palpitation and dyspnea. His past medical history was not remarkable. Family history was nonspecific. On arrival, blood pressure was 98/55 mmHg, pulse rate 140 bpm, and respiration rate 22 per minute. Heart sound was regular but rapid and the intensity of the first heart sound at the apex was variable. Fine crackles were audible in the lower lung.
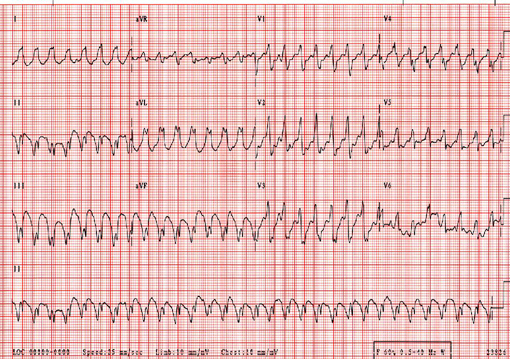
ECG taken on admission showed regular rapid rhythm with abnormal QRS complexes (Figure 1). Amiodarone 150 mg was administered intravenously, resulting in abrupt termination of the tachycardia. After restoration of sinus rhythm, 2-dimensional echocardiography revealed left ventricular dilatation (6.8 cm at end-diastole; 5.8 cm at end-systole) and global hypokinesia with ejection fraction of 38%.
|
 Legend Legend
| Fig. 1.Wide QRS complex tachycardia on arrival. Tachycardia cycle length is 320 msec. QRS complexes show left bundle branch block pattern with fatty r wave (duration: 80 msec) and prolonged RS time (>100 msec) in V1, suggesting ventricular tachycardia. In addition, AV dissociation is seen in leads I, II, and V1. Based on these findings, the wide QRS tachycardia in this case was diagnosed as ventricular tachycardia. |
 |
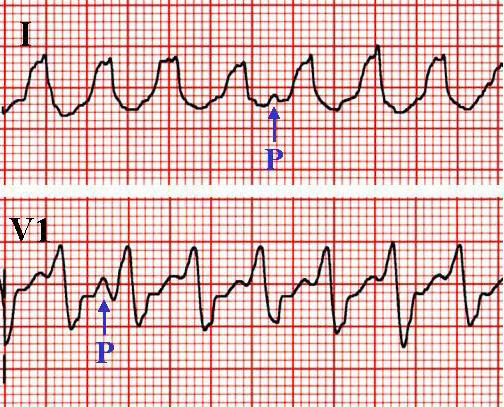
| Fig 2. Atrioventricular dissociation during the wide QRS complex tachycardia. Sinus-looking P waves are occasionally seen in leads I and V1. This finding confirmed the diagnosis of ventricular tachycardia. |
 |
In summary, dilated cardiomyopathy was complicated with sustained ventricular tachycardia showing typical QRS morphology of VT with left bundle branch block pattern.
자료제공: 전남의대 조정관 [ chojg@unitel.co.kr ]
☞ 질문이나 의견이 있으시면 회원들의 공간
 에 글을 써주시기 바랍니다 에 글을 써주시기 바랍니다
|