 Successful Optical Coherence Tomography-guided Percutaneous Coronary Intervention in Patient with Recanalization of Organized Thrombi in Proximal Left Anterior Descending Coronary Artery Successful Optical Coherence Tomography-guided Percutaneous Coronary Intervention in Patient with Recanalization of Organized Thrombi in Proximal Left Anterior Descending Coronary Artery |
|
| Treatment of Recurrent In-stent Restenosis and Stent Thrombosis After Successful Percutaneous Coronary Interventions Using Everolimus-eluting Stents in Left Main Stem Bifurcation Disease |
| Jae Yeong Cho, MD, Doo Sun Sim, MD, PhD, Young Joon Hong, MD, PhD, Hae Chang Jeong, MD, Keun-Ho Park, MD, PhD, Ju Han Kim, MD, PhD, YoungkeunAhn, MD, PhD, FACC, FSCAI, and Myung Ho Jeong MD, PhD, FACC, FAHA, FESC, FSCAI |
|
A 66-year-old woman presented with chest pain at rest lasting for 7 hours. She had a history of hypertension and dyslipidemia. Her vital signs were: blood pressure 130/80 mmHg, pulse rate 76 beats per minute, respiratory rate 20 breaths per minute, and body temperature 36.1℃. Her electrocardiogram (ECG) at admission showed normal sinus rhythm with anterior ischemia (Figure 1). Cardiac troponin-I level was elevated up to 0.77 ng/ml. Two-dimensional echocardiogram revealed akinesia in anterior wall with preserved left ventricular (LV) systolic function (ejection fraction=62%). Coronary angiography (CAG) demonstrated significant stenosis in the distal left main stem (LMS) with involvement of the proximal left anterior descending coronary artery (LAD) and the proximal left circumflex coronary artery (LCX), and significant stenosis in the LCX obtuse marginal branch (Figure 2). At the request of the patient and her family, percutaneous coronary intervention (PCI) was performed using a 7-French CLS 3.0 guiding catheter (Boston Scientific, Maple Grove, MN, USA). First, balloon angioplasty was done in the LMS, proximal LAD, proximal LCX, and LCX obtuse marginal branch using a 2.0 mm balloon. Stenting was performed in the proximal LCX using 3.0*15 mm everolimus-eluting stent (EES) at 14 atm (Figure 3A). And then, a second stent (3.0*28 mm EES) was deployed in the LMS to proximal LAD at 15 atm by the T-stenting technique (Figure 3B). The procedure was finalized with kissing balloon angioplasty with a 3.0 mm balloon in the LAD and a 2.5 mm balloon in the LCX at 6 atm, respectively (Figure 4). After procedure, she has been symptom-free with conventional dual antiplatelet therapy. Six months later, however, she presented with severe squeezing nature chest pain. In the emergency department her ECG demonstrated ST-segment depression in the anterolateral leads. Emergent CAG showed thrombus-containing near-total occlusion in the proximal stented LAD, compatible with late stent thrombosis (Figure 5A). Balloon angioplasty was performed using a 3.0 mm balloon several times with restoration of TIMI III antegrade flow (Figure 5B). Platelet function testing revealed 535 aspirin reaction units and 179 P2Y12 reaction units. Given that she developed late stent thrombosis while on conventional dual antiplatelet therapy, the subscription of antiplatelet agent was switched from clopidogrel 75 mg to prasugrel 10 mg daily and discharged after an uneventful recovery. However, 3 months later, the patient presented with chest pain from a day before and underwent follow-up coronary angiogram. An elective CAG revealed ISR in stented LM to p-LAD, de novo stenosis in m-LAD (B2, 90%, II, 0), and critical stenosis in p-LCX (B2, 95%, II, 0) (Fig 6, A). Balloon angioplasty using 2.0 mm balloon for p-LCX and 3.0 mm balloon for m-LAD was performed (Fig 6, B). Thereafter 3.0 x 18 mm EES was deployed in m-LAD due to residual stenosis. After that, plaque rupture developed in m-LAD, so 3.0 x 12 mm EES was implanted in the target lesion. Final angiography displayed good patency of LAD artery. Two months has passed and most recently, she developed chest pain again for 3 hours before presentation in emergency room. Her ECG showed ST-segment depression in V3-4 leads with elevated troponin-I of 0.37 ng/ml. CAG showed no ISR in m-LAD and moderate ISR in LM to LAD stents, but significant type II ISR in LCX stent (85%, III). No change in total occlusion of D1 branch with collaterals from RCA (Fig 7, A). After wiring in LAD and LCX, PTCA was done in LCX using a 1.0 mm and a 2.5 mm balloon, followed by drug-eluting balloon angioplasty using a 2.5*20 mm Sequent Please balloon at 10 atm (Fig 7, B). The procedure was finalized with kissing balloon angioplasty with a 2.5 mm balloon in the prox LAD and a 2.5 mm balloon in the prox LCX with good angiographic results.
|
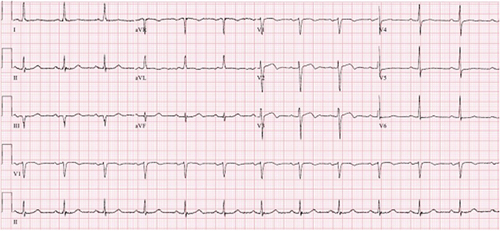 |
▲ Figure 1. Electrocardiogram at admission showed normal sinus rhythm with anterior wall ischemia.
|
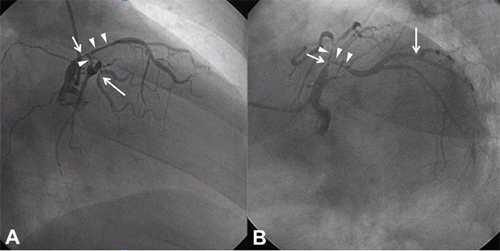 |
▲ Figure 2. Coronary angiogram showed significant stenosis in the distal LMS (short arrow) bifurcation (arrowheads) involving the proximal left anterior descending coronary artery (LAD) and the proximal left circumflex coronary artery (LCX), and significant stenosis in LCX obtuse marginal branch (long arrow). A: Right anterior oblique cranial view, B: Left anterior oblique caudal view.
|
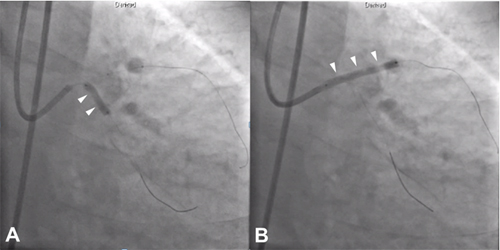 |
▲ Figure 3. Stenting was performed in the proximal LCX using a 3.0*15 mm EES at 14 atm (A, arrows) and a 3.0*28 mm EES at 15 atm by the T-stenting technique (B, arrows). A, B: Anteroposterior caudal views.
|
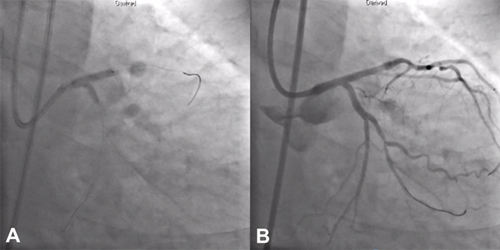 |
▲ Figure 4. The procedure was finalized by kissing balloon angioplasty with a 3.0 mm balloon in the LAD and a 2.5 mm balloon in the LCX at 6 atm, respectively (A) with good angiographic results (B). A, B: Anteroposterior caudal views.
|
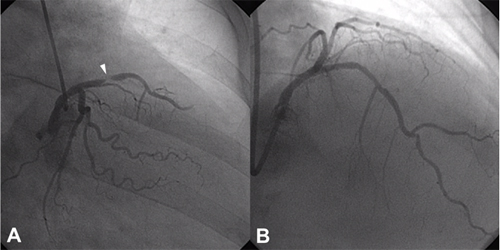 |
▲ Figure 5. Emergent CAG revealed thrombus-containing near-total occlusion in the proximal stented LAD (A, arrowhead). Balloon angioplasty was performed using a 3.0 mm balloon several times with restoration of TIMI III antegrade flow (B).
|
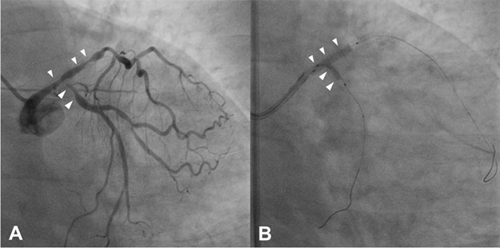 |
▲ Figure 6. Elective CAG revealed ISR in LM to m-LAD stent, de novo stenosis in m-LAD, and critical stenosis in p-LCX(A, arrowheads). After POBA for p-LCX and LAD (B, arrowheads), 3.0 x 18 mm EES was deployed in m-LAD.
|
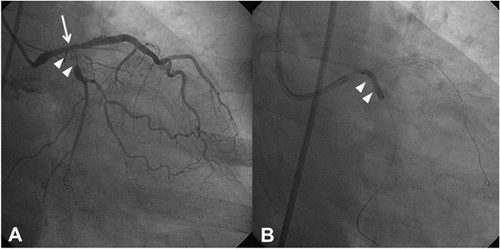 |
▲ Figure 7. Elective CAG showed significant type II ISR in LCX stent (A, arrowheads) and moderate ISR in LM to LAD stents (A, long arrow). DEB was applied to LCX ISR (B, arrowheads).
|
|
| |
위의 이달의 중재술을 보신 선생님들의 의견을 아래의 의견 쓰기에 의견을 남겨 주십시오.
선생님들의 다양한 의견을 받습니다.
|
![[의견쓰기]](/image/comment_btn.gif) |
Warning: include(/home/virtual/circulationadmin/new/info/comment_index.php) [function.include]: failed to open stream: No such file or directory in /home/virtual/circulationadmin/new/info/case/201302/case201302.htm on line 167
Warning: include() [function.include]: Failed opening '/home/virtual/circulationadmin/new/info/comment_index.php' for inclusion (include_path='.:/usr/local/php/lib/php') in /home/virtual/circulationadmin/new/info/case/201302/case201302.htm on line 167
|
|
|