Epidemiology 2
Regional Difference in Cardiovascular Mortality

Eunji Kim, MD.,PhD.
Gachon Univ Univ., KoreaCardiovascular disease (CVD) mortality has declined in recent decades, largely due to advances in prevention, medical technology, and emergency care. Deaths from myocardial infarction and stroke decreased markedly, yet these conditions remain major contributors, while heart failure is emerging as a growing challenge.
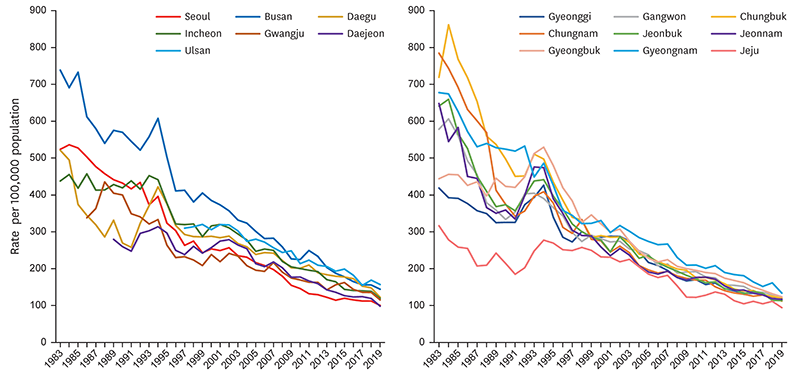
Progress has not been uniform across regions. Between 1983 and 2019, regional disparities in CVD mortality were widest in the 1980s but gradually narrowed. Still, Busan, Ulsan, and Gyeongnam consistently showed the highest mortality, while Jeju maintained the lowest, underscoring persistent inequalities. Urban–rural contrasts add complexity: nationwide, 30-day mortality after myocardial infarction and stroke declined, but rural areas saw smaller reductions and, in some cases, increases. When urban areas were further stratified, metropolitan cities other than Seoul and Gyeonggi exhibited the highest mortality, followed by smaller cities and rural areas, whereas Seoul and Gyeonggi showed the lowest rates.
These disparities are shaped by multiple factors. Although optimal distribution of healthcare resources is essential, broader determinants also play a critical role. Socioeconomic deprivation, for example, exerts a substantial influence: regions with higher deprivation indices demonstrated significantly elevated premature mortality, with the most disadvantaged facing a 41.6% greater risk. Notably, this association persisted even after adjusting for geographic access to healthcare facilities and was more evident in metropolitan areas. Lifestyle patterns also differ regionally. Analysis of the 2013–2016 Korea National Health and Nutrition Examination Survey found that rural residents consumed fewer fruits and less calcium, more sodium, and had poorer diet quality. They also exhibited higher rates of obesity, metabolic syndrome, and smoking, with CVD prevalence of 35.6%. Meanwhile, they reported more participation in physical activity than their urban counterparts, reflecting heterogeneous health behaviors rather than a simple urban–rural divide. Recent studies further highlight the role of environmental and climatic factors—including air pollution, extreme heat, and green space availability—in shaping cardiovascular risk, thereby offering insights into regional disparities in CVD burden.
Korea has achieved substantial progress in reducing the CVD burden. However, persistent regional disparities suggest that uniform national policies alone are insufficient. To achieve equitable cardiovascular health, strategies must be regionally tailored, incorporating lifestyle modification, strengthened care systems, fair resource allocation, and environmental management.