JCS-KSC Joint Session (Echocardiography)
Grading TR: Making the New Classification Work in Daily Practice

Masaki Izumo, MD, PhD.
St. Marianna University, JapanFor decades, the tricuspid valve has been referred to as the “forgotten valve.” Unlike the aortic or mitral valves, it has often received less attention in both research and clinical practice. However, mounting evidence has made it increasingly clear that tricuspid regurgitation (TR) is not a benign finding but rather a significant determinant of poor prognosis across a wide spectrum of cardiovascular diseases. In our rapidly aging societies, the prevalence of TR is steadily increasing. Elderly patients frequently present with multiple comorbidities, atrial fibrillation, or pulmonary hypertension, all of which contribute to the burden of TR. For many years, treatment options for significant TR were limited, as surgical repair or replacement carried high procedural risk and was often deferred until late disease stages. This therapeutic gap is now beginning to close. In recent years, less invasive transcatheter therapies for TR have been developed, and early experiences from clinical studies and registries have demonstrated their safety and efficacy. The accumulating evidence is shaping a new era in the management of the forgotten valve.
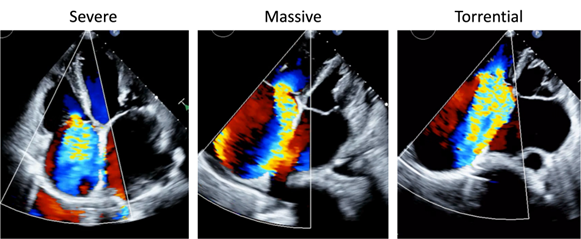
Despite these advances, the evaluation of TR severity remains a critical cornerstone of patient care. Traditionally, echocardiography has been the primary tool for grading TR, but conventional classifications were often limited to “mild, moderate, and severe.” This framework did not fully capture the wide clinical spectrum of disease, especially at the higher end. To address this gap, a new five-grade classification has recently been proposed and increasingly adopted: mild, moderate, severe, massive, and torrential TR. This extended classification allows clinicians to better stratify patients, to appreciate the incremental risk associated with extreme TR, and to define more appropriate thresholds for intervention. In daily practice, however, applying this new classification requires both knowledge and caution. Echocardiographic parameters such as vena contracta width, effective regurgitant orifice area, and regurgitant volume must be carefully integrated with supportive signs, including right atrial and ventricular remodeling, hepatic vein flow reversal, and inferior vena cava dilatation. In this session, we will focus on these practical issues. We will highlight the clinical significance of the five-grade system (figure), illustrate how it has already influenced patient selection for emerging transcatheter therapies, and discuss its impact on daily decision-making. In addition, we will address potential pitfalls, including over- or underestimation of severity, and emphasize the importance of integrating clinical context, right ventricular function, and patient symptoms alongside echocardiographic grading.
The forgotten valve is no longer forgotten: TR is now recognized as one of the major player in cardiovascular outcomes, and accurate grading is the first step toward improving the care of this growing patient population.