Echocardiography 6
Master Chef's Secret Recipe for HFpEF: The Art of Medical Therapy Using Cardiac Imaging

Jong-Won Ha, MD, PhD
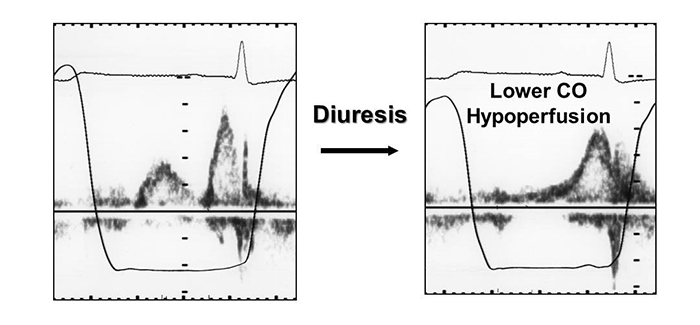
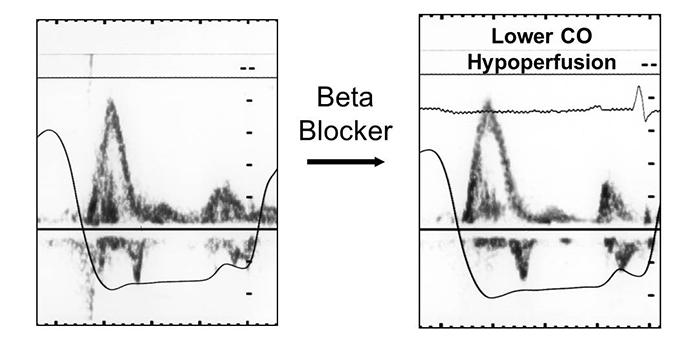
Yonsei Univ., KoreaCardiovascular disease is the most common cause of morbidity and mortality in the elderly, and heart failure is the most common hospital discharge diagnosis in this population and is still increasing. More importantly, it also has been shown that heart failure with preserved ejection fraction increases in incidence with age. Diastolic dysfunction, which can precipitate heart failure and determine prognosis, is often unrecognized and has therapeutic implications distinct from those associated with systolic dysfunction. Determination of diastolic function is an integral part of an echocardiographic examination, especially in patients with symptoms of heart failure. In an aging society, elderly patients with high rates of comorbidities are common, but determining which symptoms are attributable to cardiac conditions versus other coexisting comorbidities can be clinically challenging. Performing echocardiography in all hemodynamically unstable patients can help to guide real-time decisions regarding fluids status and evaluate treatable underlying causes of shock. Therefore, echocardiography should be performed in patients with hemodynamic instability to identify underlying treatable causes and to help guide fluid resuscitation. In this regard, understanding the mechanism and hemodynamics of diastolic dysfunction in critically ill patients is crucial. Increased understanding and assessment of diastolic function will put physicians in a better position not only to diagnose diastolic dysfunction or heart failure, but also to manage it more effectively. To optimize this approach, assessing diastolic function at the time of hemodynamic compromise or symptomatic deterioration is essential. When the preload of the heart is already high, volume expansion can be hazardous, especially in elderly patients with decreased left ventricular compliance. Because of this concern, despite the need for adequate fluid balance, dehydration in elderly critically ill patients who are admitted to the intensive care unit is not uncommon but usually unrecognized. It is important to avoid hypovolemia in these patients because it can lead to subsequent unexpected complications, such as hypotension and renal failure. Close monitoring is needed in patients being treated with volume expansion because of the delicate balance between excessive pulmonary congestion and reduced preload. Although diuretics are appropriate for the relief of congestion and edema, they are most effective in patients with evidence of fluid retention. In addition, caution should be taken to avoid overdiuresis, which may result in intravascular volume depletion and resultant hypotension or prerenal azotemia. Unlike in patients with grade 2 or 3 diastolic dysfunction (with elevated filling pressures) in whom the addition of diuretics should be considered due to elevated filling pressures, patients with grade 1 diastolic dysfunction (abnormal relaxation) will not benefit from diuretic therapy because their filling pressure is usually not elevated at rest. Echocardiographic evaluation can identify those patients who would benefit from diuresis. If there is no overt evidence of volume overload, then diuretics should not be used. Beta-blockers have been shown to reduce mortality and improve quality-of-life in patients with heart failure. However, the individual response to beta-blocker therapy is highly variable in terms of tolerance and efficacy. In patients with a restrictive physiology, because most of the filling of the left ventricle occurs in early diastole, prolonging the diastolic filling time would not be beneficial and may even be harmful due to the decrease in cardiac output as a result of the decrease in heart rate. Therefore, prolonging the diastolic filling time with a beta blocker in the presence of restrictive physiology would not be beneficial and could even be harmful.